Empowering employees with strength, adaptability, and vitality, to support a thriving personal and professional life.
Expert-led corporate wellbeing initiatives, events and training for a healthy and high-performing workplace.
Your Trusted Partner in Workplace Health & Wellbeing


Supporting mental and physical wellbeing at work isn’t just important—it’s essential for attracting top talent and driving productivity.
That’s where Thrive4Life comes in. We deliver comprehensive wellbeing initiatives, events, and training that create lasting change.
By addressing key pillars of wellbeing like nutrition, exercise, mental health, and social connection, we equip employees with the tools to stay strong, adaptable, and healthy. Our practical approach helps teams tackle challenges, reduce stress, and thrive—at work and beyond.
A Multidisciplinary Team of Health and Wellbeing Experts.
Our team is made up of specialists from every corner of the health and wellbeing world: medical consultants, surgeons, corporate psychologists, and health and wellbeing experts in their field.
Whether you need engaging workshops, in-house talks or tailored learning and development training, Thrive4Life will design bespoke solutions that seamlessly align with your organisation’s unique culture and goals.
What solutions would work for your teams?
Discover more about our health and wellbeing services and how we can tailor these for you.
DISCOVER OUR SERVICES

.jpg?updated=1761752717)
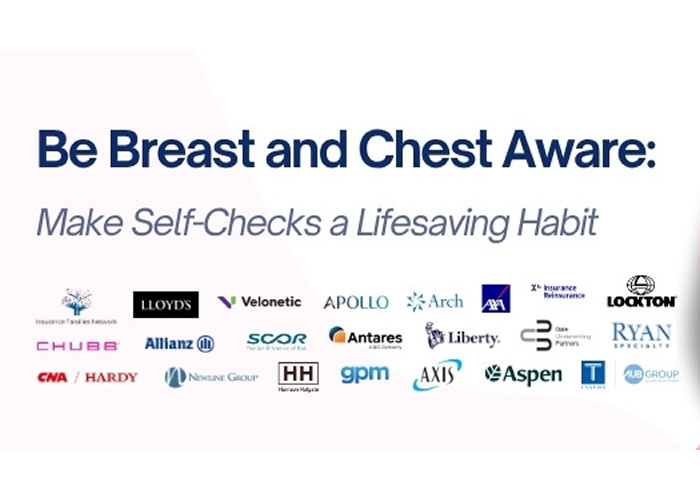
EVENT RECAP:
Be Breast & Chest Aware - Make Self-Checks a Lifesaving Habit
This October, the city came together with Lloyd’s Market for one of the largest city-wide health campaigns ever: "Be Breast & Chest Aware: Make Self-Checks a Lifesaving Habit."
Around 100 attendees joined us in-person at the Old Library, enjoying a complimentary buffet, networking with fellow professionals, and expert insights from Consultant Breast Cancer Surgeon Miss Joanna Franks. Several days later, the live webinar talk by Miss Franks reached an audience of nearly 350 people.
⟵ Watch the event highlight reel
Health and Wellbeing Services
Helping you develop and implement a health and wellbeing strategy throughout your organisation.

Ready to Activate your healthier, happier,
more productive workplace?
Thrive4Life offers a comprehensive range of services including workshops, exercise classes, talks, learning and development training courses, through to complete health and wellbeing initiatives.
Book a consultation with one of our health and wellbeing consultants to explore the tailored services and packages we can provide for your organisation.
BOOK A CHAT

Building, Supporting, and Retaining a
High-Performance Workforce.
Managing a high-performing workforce can be complex but Thrive4Life makes it simpler, by:
- Boosting Productivity: Delivering health and wellbeing programmes that tackle absenteeism and presenteeism by enhancing employee physical and mental health, reducing workplace stress, and encouraging a more engaged and effective workforce.
- Retaining Top Talent: Delivering tailored health and wellbeing solutions, such as workshops, talks, and training. Our aim is to prioritise employee wellbeing, enhance morale, and improve job satisfaction, helping organisations reduce turnover, aid in recruitment, and retain their most valuable talent.
- Driving Employee Engagement: Developing effective strategies, including training teams of Health and Wellbeing Champions, Mental Health First Aider’s and educating leaders, to cultivate a culture of health and wellbeing.
Organisations are increasingly recognising the value of genuine health initiatives and their impact on productivity, engagement, and retention. Managing a high-performing workforce can be complex, but Thrive4Life simplifies it with practical health and wellbeing solutions.
Are you ready to transform your workplace?
With Thrive4Life’s customised health and wellbeing solutions—enhancing productivity, engagement, and retention has never been simpler.
CONTACT US NOWWhy Thrive4Life?
Health and wellbeing programmes often fall short—they fail to address the unique needs of your organisation, lack actionable takeaways to enhance employee performance, and rarely provide lasting, impactful results. Thrive4Life stands apart by delivering expert-led, prevention-focused solutions with practical outcomes, all supported by exceptional ongoing service.
- Expert-Led and Evidence-Based Solutions: Thrive4Life gives you access to experts in health and wellbeing, including high-level medical consultants, ensuring your employees benefit from credible, impactful strategies.
- Practical and Cost-Effective Programmes: Our talks, training, and workshops are designed to deliver actionable takeaways employees can implement immediately, making workplace wellbeing a smart and affordable investment.
- Exceptional Customer Support: From initial consultation to ongoing delivery, we provide dedicated, reliable support to ensure your health and wellbeing initiatives achieve lasting success.
- Prevention-Focused Approach: We prioritise proactive health and wellbeing to address potential challenges before they arise, helping you build a healthier, more resilient workforce.
With over 15 years of experience in delivering health and wellbeing strategies, our senior consultants bring expertise from a variety of industries. Their knowledge ensures you receive trusted expert advice, and practical, actionable recommendations tailored to your organisation's needs.

Let’s create a healthier workplace
Why not book a call with one of our consultants to discuss how we can help you achieve your companies health and wellbeing goals?
BOOK A CHAT
Powerful Health and Wellbeing Talks to Manage Health and Wellbeing
Join us for one of our Health and Wellbeing talks which cover anything from wellbeing, mental health and mindfulness, to clinical topics including symptoms of diabetes and reducing your risk of cancer.

Webinar: Men’s Health Matters: What Really Counts – and When to Take Action
This Movember, join mental health educator Ross Abbott as he explores the silence around men’s mental health and how we can all play a role in changing the conversation.
- Wednesday 19 November 2025
- 1:00 pm - 1:30 pm

In-Person Talk: Feed Your Immune Defences This Winter - Five Essential Nutrition Tips
Join Lissa Leader, Registered Nutritionist, to uncover how gut health, the microbiome, and smart nutrition choices can help to support your immune system and keep you feeling your best this winter.
- Tuesday 09 December 2025
- 1:00 pm - 1:30 pm
- Cost: £5

Webinar: Feed Your Immune Defences This Winter - Five Essential Nutrition Tips
Join Lissa Leader, Registered Nutritionist (MBANT), to uncover how gut health, the microbiome, and smart nutrition choices can help to support your immune system and keep you feeling your best this winter.
- Thursday 11 December 2025
- 1:00 pm - 1:30 pm
Webinar: Your Best Year Yet - A Psychologist's Guide to Creating Habits That Last
Make 2026 your year of change! Join Chartered Senior Psychologist Kate Busch to uncover the science of habits and learn simple, practical strategies to build routines that stick.
- Tuesday 20 January 2026
- 1:00 pm - 1:30 pm

In-person Talk: Your Best Year Yet - A Psychologist's Guide to Creating Habits That Last
Make 2026 your year of change! Join Chartered Senior Psychologist Kate Busch to uncover the science of habits and learn simple, practical strategies to build routines that stick.
- Thursday 22 January 2026
- 1:00 pm - 1:30 pm
- Cost: £5
Read our Latest Health Insights
With so many wellbeing experts and health specialists in our network, we’re keen to share what we can with you!
Take a look at our latest articles, blogs and ultimate guides.
Why not sign up to our health and wellbeing emails so you’re up to date with up and coming Thrive4Life news and events.
Click the button below to complete the form and receive regular emails to help you manage your health and wellbeing.
subscribe